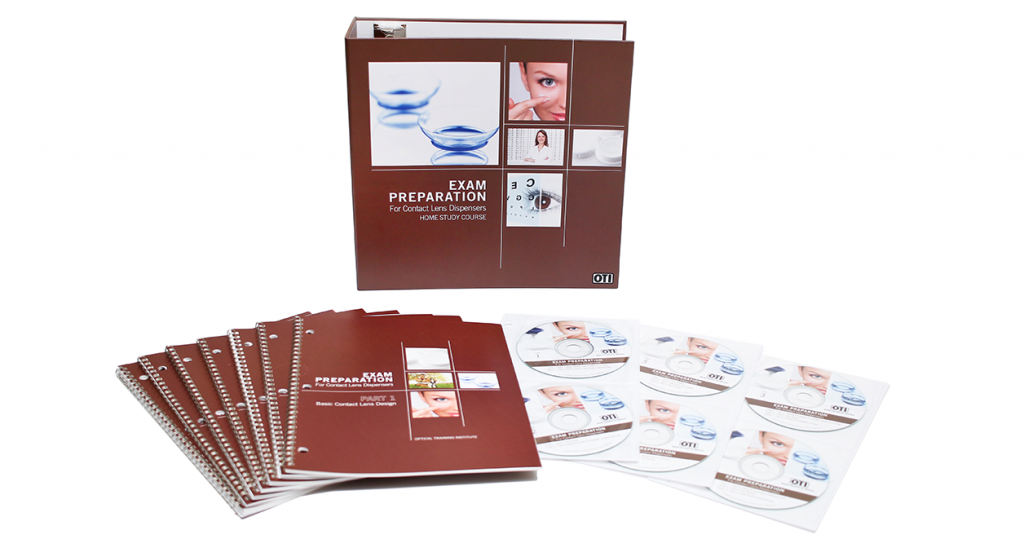
Six workbooks and audio tracks work together to logically and concisely cover every subject, with explanations, tables, charts, diagrams, exercises, and over 150 practice test questions. Audios are available online and included as six CDs.
ORDER NOWWhat You Will Learn from This Course
Covers the various contact lens designs to include scleral, corneal and semi-scleral designs. Some basic terminology is discussed and the various materials from which contact lenses can be made are surveyed and placed into historical perspective. The uses, advantages and disadvantages of the lens materials are covered. The parts of a contact lens are covered to include, optic zone, peripheral curve, base curve, junction zone, and radius of curvature. The need for diopter to millimeter conversion is covered and a table is included. This course also includes a discussion of the relationship between sagitta depth and fit. Changing sagitta depth by manipulating lens diameter and /or base curve radius is presented. A brief glossary of the terms covered concludes the section.
This section covers basic principles of optics which must be considered when fitting rigid and soft contact lenses. It includes a discussion of vertex distance as well as the optical effects of the lacrimal lens which is formed between the front surface of the cornea and the back surface (base curve) of the lens. Examples and practice exercises are included to cover instances of rigid lenses fit on K, steeper than K, and flatter than K. This course also covers patient selection. Through the use of appropriate prefit testing and interviewing techniques, an attempt is made to identify contact lens candidates with the best prognosis for successful wear as well as those with a reduced prognosis. A review of certain anatomical features of the eye is included with an emphasis on the structure of the tear film and the cornea.
The various fitting philosophies of rigid and soft lenses are presented. Although PMMA lenses are rarely fit today, the basic principles of fitting them are fundamental to all rigid lenses and are therefore covered in this section. It includes discussions of palpebral lenses as well as larger lenses with wider peripheral curves. The general characteristics, advantages, and disadvantages of each are discussed. Methods and procedures for selecting base curve, diameter, optical zone width, peripheral curves, and thickness are covered to include the use of nomograms and diagnostic lenses. Dynamic flourescein patterns used to assist in the evaluation of the fit of rigid lenses are discussed. These include spherical base curves on spherical corneas as well as spherical base curves on toric corneas. Astigmatism with the rule, against the rule, and oblique will be discussed and observed. Soft lens evaluation is then covered to include fitting goals and the characteristics of a good fitting soft lens. The course concludes with a presentation of rigid and soft lens verification techniques to include the hand magnifier, diameter gauge, projector inspection devices, slit lamp, radiuscope, thickness gauge, lensometer, and profile analyzer.
This section begins with a review of certain anatomical structures which include the tear film, eyelids, conjunctiva, cornea, and limbus. It is followed by a discussion of some of the potentially adverse effects of contact lens wear such as corneal edema, corneal striae, conjunctiva and episcleral injection, giant papillary conjunctivitis, corneal vascularization. Corneal epithelial staining patterns are then discussed and illustrated to cover those caused by direct trauma such as by a poorly edged or damaged lens, or by improper insertion, removal and recentering techniques. Also covered are staining patterns caused by defective tear film distribution over the cornea such as “three and nine-o-clock” staining. Part 4 concludes with a discussion of the biomicroscope or slit-lamp, emphasizing its importance in the fitting of contact lenses.
This section covers the use of contact lenses for the correction of presbyopia, astigmatism, aphakia, and keratoconus. While the fitting of contact lenses for any of these conditions requires a great deal of skill, the basic principles and philosophies employed will be presented. These include the utilization of the monovision technique as well as the use of concentric and segment style bifocal lenses for the correction of presbyopia. Techniques for inhibiting lens rotation are covered to include prism ballast, truncation, toric surfaces, and double slab-off. Front toric, back toric and bitoric contact lenses and their application for the correction of astigmatic conditions will be covered. Lenses for the correction of aphakia include conventional lenticular designs as well as minus carrier lenticulars, and single cut lens designs. This section will conclude with a discussion of keratoconus, describing contact lens fitting methods and philosophies.
This final section of the home study course begins with a description of in- office modifications that are possible with rigid contact lenses. Included among these are the reduction of lens diameter, blending transition zones, removing scratches, adding minus power and dotting the lens for identification. The use of the radiuscope is described and illustrated as it is used to verify the radius of curvature of a spherical surface. This section continues with a discussion of the various solutions for rigid and soft lenses. These include wetting, cleaning, and soaking solutions for rigid lenses, and cleaning disinfecting, rinsing, and re-wetting solutions for soft lenses. Thermal and chemical disinfection for soft lenses is discussed followed by a presentation of patient instruction techniques for lens insertion and removal. Following a discussion of ANSI standards for contact lenses, Part 6 concludes with a glossary of terms which were presented and used throughout the course.
Choose one of the best preparation courses, which is proven to increase your chances of passing the exam on your first try.
ORDER NOW