
Components and Design of the Slit Lamp
The slit lamp’s design integrates several key components that work in harmony to facilitate detailed ocular examination. The slit lamp or biomicroscope is an instrument designed primarily to observe the transparent structures of the human eye under a magnification of between 10 to 50 times. Its two principal parts include a lamp equipped with an optical system designed to project a slit of light upon the eye, and a stereomicroscope which is mounted horizontally for direct viewing of the patient’s eye. The slit lamp may be adjusted to project a variety of light beams. By varying the light beam and the viewing position, it is possible to improve the view of the various structures of the eye. Since the biomicroscope is particularly useful for examining the cornea, it plays an especially important role in the fitting of contact lenses. Symptoms of a poor-fitting contact lens, for example, can usually first be detected through the use of the slit lamp.
Understanding these elements is essential for optimal utilization of the instrument. This is also an integral topic covered in the ABO-NCLE exam.

Illumination System
At the heart of the slit lamp is its illumination system, which produces a high-intensity beam of light. This system typically consists of:
- Light source: Usually a halogen or LED bulb
- Condensing lenses: Focuses the light into a beam
- Adjustable slit aperture: Controls the width and height of the light beam
- Filters: Modify the spectral characteristics of the light
The illumination arm can be rotated around a central pivot, allowing the examiner to direct light from various angles. This flexibility is crucial for employing different illumination techniques.
Observation System
The observation system comprises a binocular microscope that provides stereoscopic magnification of the eye. Key features include:
- Eyepieces: Adjustable for individual interpupillary distance and refractive error
- Objective lenses: Offer various magnification levels, typically ranging from 6x to 40x
- Focusing mechanism: Allows fine adjustment of the focal plane
The microscope is mounted on a swivel arm, enabling the examiner to align it with the illumination beam and achieve optimal viewing angles.
Patient Support and Positioning
To ensure stability during examination, the slit lamp incorporates:
- Chin rest: Supports the patient’s head
- Forehead rest: Minimizes head movement
- Height-adjustable table: Accommodates patient height
Proper patient positioning is crucial for maintaining the eye within the instrument’s focal range throughout the examination.
Control Mechanisms
Various controls allow the examiner to manipulate the instrument:
- Joystick: Enables fine movements in horizontal and vertical planes
- Magnification selector: Switches between different magnification levels
- Slit width and height adjusters: Modify the dimensions of the light beam
- Filter selection lever: Chooses appropriate light filters for specific examination techniques
Mastery of these controls is essential for efficient and thorough examination.
Illumination Techniques in Slit Lamp Examination
The slit lamp’s versatility stems from its ability to employ various illumination techniques, each offering unique advantages in visualizing different ocular structures.
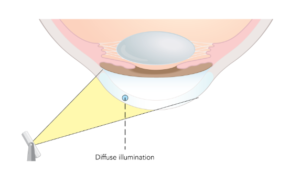
Diffuse Illumination
This technique provides a broad, overall view of the anterior segment:
- A wide beam of light is directed obliquely at the eye
- This beam is useful for a general survey and assessment of gross abnormalities
- Ideal for examining the conjunctiva, sclera, and external adnexa
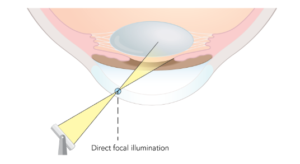
Direct Focal Illumination
Direct focal illumination techniques offer detailed views of specific ocular structures:
- Optical Section:
- A narrow, intense beam is focused on the cornea
- Provides a cross-sectional view of corneal layers
- Useful for assessing corneal thickness and detecting abnormalities
- Parallelepiped:
- A wider beam is used to illuminate a rectangular area
- Facilitates examination of the corneal surface and endothelium
- Valuable in contact lens fitting assessment
- Conical Beam:
- A focused, cone-shaped beam is directed into the anterior chamber
- Enhances visualization of aqueous flare in cases of inflammation
These techniques allow for precise localization of pathology within the cornea and anterior chamber.
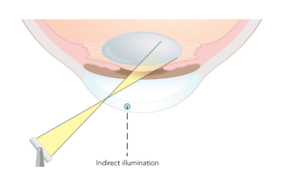
Indirect Illumination
Indirect illumination involves focusing the microscope on an area adjacent to the illuminated zone:
- Enhances contrast and visibility of subtle opacities
- Particularly useful for examining the iris and detecting foreign bodies
- Can reveal fine corneal opacities that may be missed with direct illumination
This method is invaluable for detecting subtle pathological changes in transparent structures.
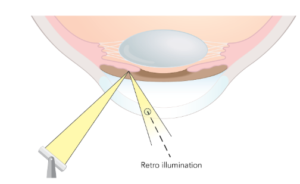
Retroillumination
In retroillumination, light reflected from deeper structures is used to examine more anterior ones:
- Reflected light from the iris or retina illuminates the cornea or lens
- Useful for detecting corneal opacities, lens vacuoles, and iris transillumination defects
- Enhances visualization of corneal neovascularization
This technique provides unique insights into the transparency and integrity of ocular structures.
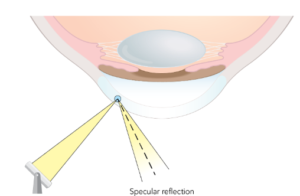
Specular Reflection
Specular reflection utilizes the mirror-like properties of smooth ocular surfaces:
- The angle of incidence of the light beam equals the angle of reflection
- Allows examination of the corneal endothelium and tear film
- Valuable in assessing contact lens fit and surface quality
Mastery of this technique is crucial for evaluating the health of the corneal endothelium.
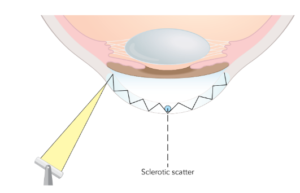
Sclerotic Scatter
A wide beam of light is directed at the temporal limbus, allowing it to pass through and illuminate the nasal limbus. Then, the microscope is precisely adjusted to focus on the cornea. This illumination type helps identify corneal edema.
Filters
Cobalt Blue Filter: Commonly used after instilling fluorescein dye to observe staining patterns and lens fit.
White Filter: Used to decrease UV rays and to minimally decrease light intensity. Primarily used for routine examination.
Neutral Density Filter: Decreases light intensity by about 10%. Used to examine eyelids and conjunctiva. Useful for photophobic patients.
Green Filter (red free): Makes red or brown objects appear blacker. Useful for observing blood vessels.
Slit Lamp Exam of the Ocular Structures
Examination of Ocular Structures
The slit lamp enables detailed examination of various ocular structures, each requiring specific techniques and considerations.
Eyelids and Adnexa
Examination of the eyelids and surrounding structures involves:
- Assessment of lid position, closure, and blink dynamics
- Evaluation of the lid margins for signs of blepharitis or meibomian gland dysfunction
- Inspection of the lacrimal apparatus and puncta
Diffuse illumination is typically employed for this part of the examination.
Conjunctiva and Sclera
The conjunctiva and sclera are best examined using:
- Diffuse illumination for overall assessment
- Direct focal illumination to detect fine abnormalities
- Lid eversion to examine the palpebral conjunctiva
Key aspects to evaluate include vascularity, pigmentation, and the presence of lesions or foreign bodies. The microscope and light beam are aligned to focus on the same specific area. Direct focal illumination can be categorized into three types: 1) optic section, 2) parallelepiped, and 3) conical beam. The optic section technique provides a detailed cross-sectional view of the cornea, allowing visualization of all its layers. This method is useful for identifying distortions in corneal shape and determining the depth of embedded foreign bodies. Parallelepiped illumination offers a wider view of both the anterior and posterior surfaces of the cornea. It is commonly used to evaluate surface irregularities and to examine the corneal endothelium. This technique is often paired with fluorescein dye to assess the fit of a contact lens. The conical beam technique is highly sensitive for detecting flare or increased reflectivity in the anterior chamber’s aqueous humor. When observed under high magnification, it creates the appearance of light cutting through fog, making it particularly effective for detecting subtle changes in clarity.
Cornea
Corneal examination is a critical component of slit lamp biomicroscopy:
- Optical section technique reveals the layered structure of the cornea
- Specular reflection assesses the endothelium and tear film
- Fluorescein staining highlights epithelial defects
Careful scrutiny of the cornea can reveal a wide range of pathologies, from subtle dystrophies to infectious keratitis.
Anterior Chamber
Evaluation of the anterior chamber includes:
- Assessment of depth using the Van Herick technique
- Detection of cells and flare indicative of inflammation
- Examination for hyphema or hypopyon in cases of trauma or infection
The conical beam technique is particularly useful for detecting subtle aqueous abnormalities.
Iris and Pupil
Examination of the iris and pupil involves:
- Assessment of iris color, pattern, and symmetry
- Evaluation of pupil size, shape, and reactivity
- Detection of synechiae or other abnormalities
Retroillumination can reveal transillumination defects or other structural abnormalities of the iris.
Crystalline Lens
The crystalline lens is best examined after pupillary dilation:
- Direct illumination reveals opacities and nuclear sclerosis
- Retroillumination highlights cortical and posterior subcapsular cataracts
- Assessment of lens position and stability
Careful lens examination is crucial for cataract evaluation and surgical planning.
Advanced Slit Lamp Techniques
Beyond basic examination, the slit lamp can be employed for various specialized techniques.
Gonioscopy
Gonioscopy allows visualization of the anterior chamber angle:
- A special contact lens is placed on the cornea
- The angle structures are examined using the slit lamp
- Critical for diagnosing angle-closure glaucoma and other angle abnormalities
Proficiency in gonioscopy is essential for comprehensive glaucoma management.
Fundus Examination
With additional lenses, the slit lamp can be used for fundus examination:
- 90D or 78D lenses provide a wide-field view of the retina
- Useful for examining the optic nerve, macula, and peripheral retina
- Stereoscopic view allows assessment of optic nerve cupping and retinal elevation
This technique offers an alternative to direct ophthalmoscopy for posterior segment evaluation.
Applanation Tonometry
The slit lamp serves as a platform for Goldmann applanation tonometry:
- A tonometer prism is mounted on the slit lamp
- Intraocular pressure is measured by applanating the cornea
- Blue light and fluorescein are used to visualize the applanation mires
This remains the gold standard for intraocular pressure measurement.
Anterior Segment Photography
Many modern slit lamps incorporate digital imaging capabilities:
- Allows documentation of anterior segment findings
- Useful for monitoring disease progression and treatment response
- Facilitates patient education and communication with colleagues
Digital imaging enhances the diagnostic and educational value of slit lamp examination.
Slit Lamp Examination in Contact Lens Practice
The slit lamp plays a crucial role in contact lens fitting and management:
- Assessment of lens fit and movement on the eye
- Evaluation of corneal health and contact lens-induced changes
- Detection of complications such as neovascularization or infiltrates
Regular slit lamp examination is essential for ensuring safe and successful contact lens wear.
Slit Lamp Examination in Ocular Emergencies
In emergency settings, the slit lamp is invaluable for assessing:
- Corneal foreign bodies and abrasions
- Chemical burns and their severity
- Acute angle-closure glaucoma
- Hypopyon in cases of endophthalmitis
Prompt and accurate slit lamp examination can be sight-saving in these situations.
Enhancing Slit Lamp Skills
Developing proficiency in slit lamp examination requires:
- Regular practice and repetition
- Familiarity with normal variations in ocular anatomy
- Knowledge of pathological findings and their clinical significance
- Continuous education and staying updated on new techniques
Mastery of slit lamp biomicroscopy is a lifelong journey for eye care professionals.
Future Directions in Slit Lamp Technology
Advancements in slit lamp technology continue to enhance its capabilities:
- Integration of optical coherence tomography (OCT) for high-resolution cross-sectional imaging
- Automated analysis of corneal endothelial cell counts
- Incorporation of artificial intelligence for lesion detection and classification
- Enhanced digital imaging and telemedicine applications
These innovations promise to further expand the utility of the slit lamp in ophthalmic practice.
OTI Summary of Slit Lamp in 2025
The slit lamp remains a cornerstone of ophthalmic examination, offering unparalleled insights into ocular anatomy and pathology. By understanding its components, mastering various illumination techniques, and applying them systematically to examine different ocular structures, eye care professionals can harness the full potential of this remarkable instrument. As technology continues to evolve, the slit lamp will undoubtedly remain an indispensable tool in the diagnosis and management of ocular conditions, ensuring the highest standard of patient care in ophthalmology and optometry.
Enhancing Hands-On Learning with the OTI Optician Simulator
Mastering slit lamp examination is a skill that requires precision, practice, and a deep understanding of ocular anatomy. While hands-on experience is crucial, access to real-world training opportunities can be limited. That’s where the OTI Optician Simulator comes in.
- Realistic optical simulations that replicate clinical scenarios
- Interactive learning tools designed to enhance practical skills
- A self-paced, online platform for reinforcing CE course knowledge
- An ideal training solution for students, apprentices, and professionals
With the OTI Optician Simulator, opticians and eye care professionals can develop the necessary expertise in a risk-free environment, bridging the gap between theoretical learning and clinical application.
Explore the OTI Optician Simulator Here
Ready to take your optical knowledge to the next level? Stay updated with the latest industry trends, news, and updates by joining our email newsletter. Don’t miss out—subscribe today and stay ahead in your optical career!



